What Mental Health Professionals Can Do About Climate Change
This should not be our response.
What should our response be?
Start a discussion group/journal club at your institution to loop more professionals into climate-aware practices. Request one of our senior members to join and assist. Email membershipcoordinator@climatepsychiatry.org.
Register as a climate-aware therapist
Give a talk at your institution, district branch meeting, etc. We can provide materials, mentorship, guidance, and even partnership with an accomplished speaker.
Do some writing for trade journals such as Psych News, Psych Times, peer-reviewed journals, mainstream media, etc.
Green your practice: free membership in My Green Doctor to CPA members.
Donate: as with so many groups, we have meager financial resources. Your contributions go a long way to helping us grow. Consider a regular monthly or quarterly donation.
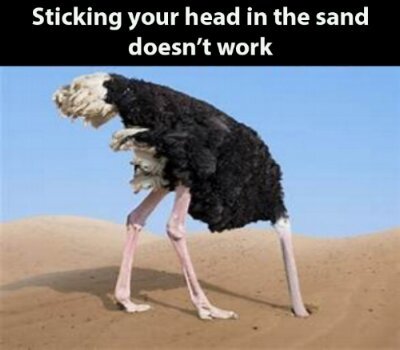
There are things that we, as professionals, can do to maximize good health outcomes for our patients, families, and communities.
Health care providers, including psychiatrists, can have an impact at multiple levels, including in how they conduct individual patient management, help develop systems of care and advocate on behalf of public health policy.
Individual Patient Management
As physicians and providers, we are the first line in keeping our patients safe and healthy during the inevitable extreme weather events and the impacts of climate change. This is a focus on direct clinical care and derives from the doctor/caregiver-patient relationship model and principles of clinical practice.
What we can do at the patient-care level:
Teaching patients and families about climate-related health risks and protective behaviors, especially regarding heat exposure and flood and storm protection in vulnerable areas
Effectively managing psychiatric medications to reduce risk
Treating specific psychiatric syndromes associated with climate-related traumas
Teaching patients and families about individual resiliency behaviors, such as transformational resilience.
Consider psychotherapeutic techniques for patients who present with eco-anxiety
Utilize colleagues and peer consultation groups, especially to reflect on secondary trauma that therapists experience and countertransference
Prepare our Agencies and Practices
Plan for closer monitoring of vulnerable populations; Engage caregivers, case managers, visiting nurses, family members, etc
Help patients, families, and staff at residential institutes and day centers develop emergency plans including plans for respite shelters during extreme weather events
Identifying what your agency/practice needs regarding health record systems and information retrieval, and operating during emergency periods
Agency and practice leaders and administrators create a culture of attention to climate-related health interventions, providing regular staff training prior to periods of greatest vulnerability and identifying roles of staff members for safety plans.
Help Develop A System of Care
This focus derives from a community mental health/public health model with attention to community and population health, safety and resiliency. Components include prevention and community preparedness as well as community disaster response and recovery. We can work to improve the readiness of community and mental health systems to respond effectively and quickly to emergencies requiring prior planning, coordination and capacity building.
How we can help at the systemic level:
Building collaborative relationships between mental health and health agencies and community groups, including public health departments, schools, churches and synagogues, recreational centers, libraries, and homeless services.
Developing systems of responsiveness: Who alerts vulnerable people/patients? What plans are in place to direct vulnerable people/patients to areas of safety?
Planning specifically for the homeless population
Supporting public health educators in developing and implementing community education strategies
Educating and coordinating with first responders (police, fire department, and local emergency departments)
Developing mental health disaster response plans and training: SAMHSA Behavioral Health Disaster Response training modules available.
Note: The scope of disaster preparedness and response may be beyond the skills of many practicing psychiatrists. All communities have Disaster Preparedness Plans usually within the Department of Public Health where useful sources of information and guidance may be found.
Training in Psychological First Aid
Providing consultation to community leaders on effective communication during acute disasters with emphasis on Psychological First Aid principles.
Training in media skills, so as to develop effective community communication